SERVICES & SOLUTIONS
A/R & Denial Management
Every day it becomes harder to get full reimbursement for laboratory claims the first time they are submitted. Both in-network and out-of-network claims come with their own unique challenges that traditional medical billing companies do not handle properly.
Get more timely reimbursements with automated laboratory denial management
![]() Eligibility checks
Eligibility checks
![]() Prior authorization
Prior authorization
![]() Claim scrubbing
Claim scrubbing
![]() Clearinghouse flexibility
Clearinghouse flexibility
![]() Customized rules
Customized rules
![]() Automated PHI entry
Automated PHI entry
3/4
of denied Medicare claims involve laboratory services.
*source: Health Payer Intelligence, 2019
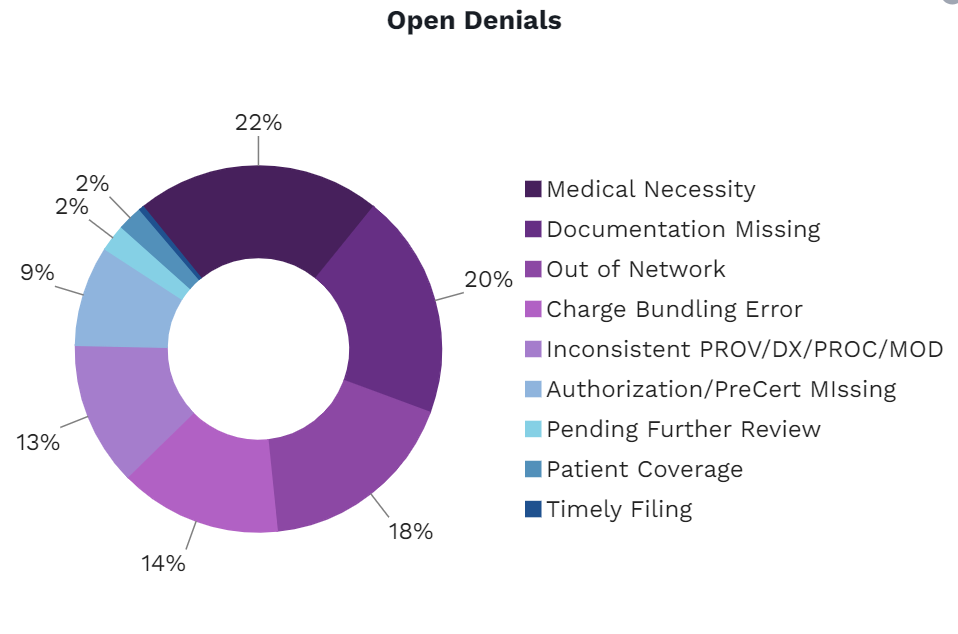
Identifying reasons for denials
We report the feedback on denied claims and display them in groups based on payer’s reason codes.
Correction and resubmission
We take the necessary measures with providers and payers to correct the claim and resubmit them properly.
Tracking and follow-up
Resubmitted claims are tracked automatically, and our team works on follow-up until the claim is successfully accepted.
Custom rule-based prevention
Our developers build custom rules to flag and correct claims that experience recurring denials before they’re sent to payers.
Less labor, less denials, more revenue for your lab
In-house billing contributes to more overhead, more manual input errors, and more denials for your laboratory. Outsourcing to our laboratory billing company will equip your lab with the most advanced automated systems that eliminate the need for manual processes and give you the insights you need to improve your clean claim rate and collect more revenue.
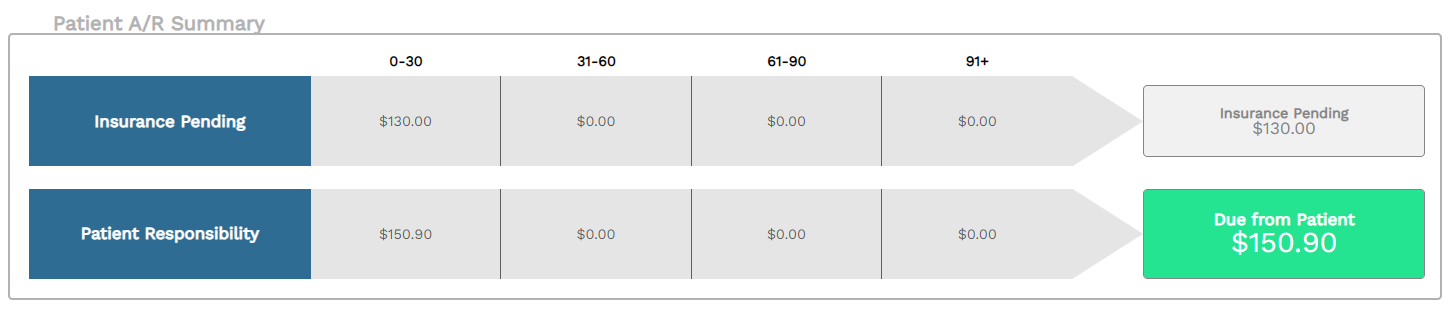
Complete transparency into the status of your laboratory claims
Take the guesswork out of correcting denials and knowing how much reimbursement is being held for different indicators. Phytest ensures every rejected claim is handled and corrected by our team of experienced, on-shore billing staff that work with patients, providers, and payers personally to get your lab the reimbursement it is owed.
A/R management made for labs
We’ve simplified the workflow and visibility into tracking your reimbursements. Drill down to the patient-level to view A/R reports broken down by length of time, payers, and more.
Our experienced lab billing staff track and follow-up rejected claims with both patients and payers giving you timely reimbursements.
Full-service laboratory revenue cycle management
Laboratory billing is unique, just like your laboratory. Our full-service revenue cycle management solutions were built specifically for promoting the growth of laboratories only. See why so many of our clients have made the switch from in-house billing and subpar medical billing companies.
Claim Scrubbing
Our AI detects and flags any inconsistencies, missing documentation, or checks unique to each lab’s circumstances.

Patient Pay
Collect payments faster by giving your patients the resources of easily accessible payment portals and live support staff.

Reporting & Metrics
Access your real-time reporting dashboard for complete transparency into your lab’s financials.